Miniature organs on chips could revolutionize health-care research
To understand how bodies work, medical researchers and scientists have created miniature models of organs, called organoids. This field of scientific research has had profound impacts on biological discovery and pharmaceutical development.
An organoid is a miniaturized version of an organ. As the name suggests with the Greek suffix oid, meaning “like,” an organoid is designed to mimic the organ it represents. These three-dimensional structures are generated from stem cells and, although only about one millimetre in size, they effectively emulate the morphology or function of the actual organs.
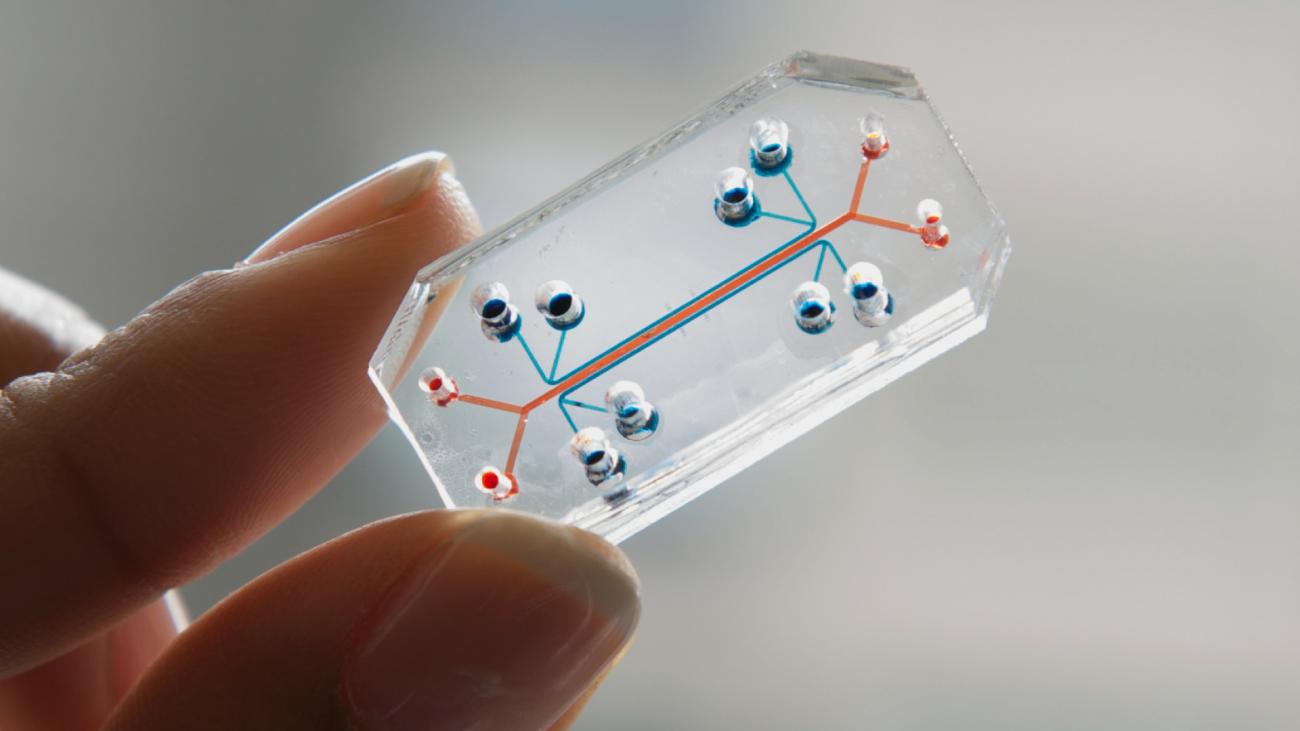
Yet this is only half the narrative. “Organs-on-chips” are a technology that uses intricately carved tunnels (microchannels) on a piece of plastic or polymer that can house cells. These channels facilitate the flow of cell culture media, replicating blood flow in the human body.
Organs-on-chips act like a miniature version of the body’s organs in the lab, making it easier to see if new drugs will work. They act as a dynamic in vitro (artificial) system to better replicate the in vivo (actual living) environment of cells.
These technologies emerged as a solution to the challenges of drug development, which is both time-consuming and exorbitantly expensive.
Safe drug development
Developing new drugs has become an arduous and costly process, requiring an average of 14 years and over US$1 billion to bring a drug to market. In addition, developing new drugs includes a high likelihood of failure.
One of the main reasons for the slow development of new drugs is the inadequate tools for accurately predicting how a drug will work in the human body. To address this, there is a growing recognition of the need for new models, such as organoids and organs-on-chips, which could revolutionize our ability to evaluate drug efficacy more effectively and efficiently.
Game-changing research
While both organoids and organs-on-chips hold individual promise, the combination of the two — “organoids-on-chips” — is a game changer. Organoids, despite their excellent biological complexity, lack certain biophysical cues, crucial for a comprehensive representation of human tissues.
On the other hand, organs-on-chips, while incorporating dynamic micro-environments, often incorporate less-than-optimal biological models. Labs often use commercially produced cell lines with genetically altered features.
By combining these technologies, we can leverage the biological accuracy of organoids with the dynamic capabilities of organs-on-chips. This synergy offers a platform that mirrors in vivo physiology, enabling a more accurate study of disease traits and responses to drugs.
In our lab, our primary focus is on incorporating a functional vascular system to organoids. A major breakthrough came in 2019 when we generated blood vessel organoids from human stem cells, providing an unprecedented model for vascular structures.
By integrating these blood vessel models into microfluidic chips and supplying them with blood, immune cells or drugs, we are paving the way for advanced organoids-on-chips that embody the necessary complexity. This enhanced vascular model enables us to vascularize a variety of biological tissues, improving their lifespan, function, growth, and maturation.
Merging physics and biology
The interdisciplinary foundation of organoids-on-chips combines biology and physics to reflect the intricate interplay of physiological and physical processes in the human body. By integrating principles from both fields, we can develop more sophisticated and accurate physiological models that encompass this inherent complexity.
The pioneering work of researchers at the Wyss Institute at Harvard University is a striking example of the potential of this interdisciplinary approach. In 2010, they developed a “lung-on-chip” model that not only mimics the biological structure of lung cells, but also replicates the mechanical function of human breathing.
In a remarkable display of innovation, they also created a smoking robot to simulate the effects of cigarette smoke on this lung-on-chip device, and tested COVID-19 drugs during the pandemic.
From its initial conception, the field of organs-on-chips has grown exponentially. Highlighting this trend, the geneticist and microbiologist Hans Clevers now leads the pharmaceutical giant Roche’s research division. “In 20 years,” Clevers said, “I think organoids will have replaced animal experimentation in toxicology testing.”
In a parallel move, Roche set up the Institute of Human Biology, under the direction of bioengineer Matthias Lutolf. The institute merges the study of organoids with microfluidic technology.
Future of organoids
A pivotal development in 2023 was the US Food and Drug Administration’s decision to no longer mandate animal testing for new drugs before advancing to human trials. This change underscores the potential of alternatives like organoids and organs-on-chips in early drug testing, and marks a significant milestone for the field.
The potential of organoids-on-chips extends beyond drug screening and toxicity tests. The technology holds promise for a range of exciting applications, including unravelling the fundamental biological principles underlying development and disease. Their applications extend to regenerative medicine, where organs grown from a patient’s own stem cells could be used to replace damaged ones.![]()
Clément Quintard is a postdoctoral fellow at the Penninger Lab at the University of British Columbia. This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()